Back in August I wrote a piece about the future of ICUs and discussed the unlikely potential of the hospital of the future being composed of a majority ICU beds. While my Magic 8 ball didn’t predict the emergence of COVID-19, it’s still “very doubtful” that on the other side of the COVID-19 curve we’ll see hospitals convert a majority of their medical/surgical beds into ICU beds. However, we do anticipate that facilities will prioritize previously planned ICU expansion projects and will reevaluate projected ICU bed need. Here are some factors to consider when reevaluating critical care capacity need.
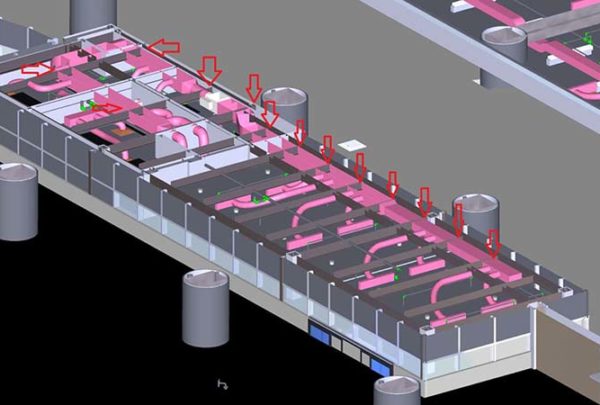
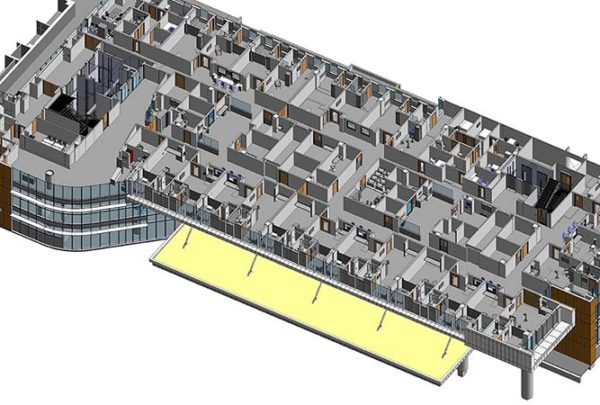
- Your patient acuity/service line mix is the linchpin behind your critical care bed need complement. Hospitals with a high percentage of cardiovascular, neurology, and general surgery cases will typically have a larger complement of critical care beds than hospitals with a high percentage of obstetrics, orthopedics, and oncology cases. Your strategic plan and provider recruitment plans could have drastic impacts on your future case mix, so before you put shovel to ground with ICU expansion, it’s important to evaluate the downstream impact these strategies will have on your overall bed complement.
- Several variables affect your inpatient average length of stay (ALOS). Where medical/surgical bed inpatient capacity is limited, it’s not uncommon to see patients boarded in ICUs longer than medically necessary. We recommend evaluating current operations and pressure-testing opportunities to reduce ALOS to capitalize on precious critical care capacity.
- While most critical care beds are (or have been converted to) private beds, it’s important to consider your mix of semi-private beds across the house. While numerous challenges are associated with semi-private beds, infection control rises to the top of the list. It goes without saying that amid our current crisis, we must evaluate the appropriate mix of semi-private beds and how to flex the current bed complement to accommodate infectious disease patients.
- When planning inpatient bed additions, replacement, and/or renovations, the topic of acuity adaptable beds frequently comes up. Some hospitals have a mix of these types of beds today; however, it is not the norm. Given the capital costs, we don’t anticipate that hospitals will be able to go this route on all future inpatient bed projects, but it’ll be important to determine the appropriate complement going forward.
Our team often uses the expression that we don’t want to “plan for Easter Sunday.” While we didn’t know that Easter Sunday 2020 would be the highest critical care volume to date for some hospitals across the country, it was also the lowest volume day for others because elective surgeries are on hold. Our teams continue to work alongside our clients, overlaying their unique hospital and market dynamics to find the right balance for the future.