Read Part 1 to learn more about how to coordinate your response to a pandemic.
The COVID-19 pandemic has exposed the vulnerabilities of the U.S. healthcare system. We as an industry must recognize our weaknesses and proactively work on closing the gaps as quickly as possible to try to avoid another socioeconomic disaster during the next wave. In Part 1 of this blog, I addressed the importance of a coordinated response to a pandemic, increasing bed capacity, and embracing guidelines for preventing infections. Just as critical are protecting your staff members at times when they’re working long hours in difficult conditions.
Can you maintain an adequate healthcare workforce during this crisis and in the future?
Recruiting, retaining, and protecting healthcare workers is foundational in sustaining the U.S. healthcare system. These workers are at the highest risk during the pandemic because of their prolonged exposure to infected patients. Inadequate protection not only undermines their ability to provide clinical care but fractures the system’s social responsibility to the community. This will require healthcare systems to not only maintain an adequate number of healthcare workers but also optimize the conditions that enable clinicians to care for a high volume of patients.
Limit staff exposure to COVID-19 patients by dedicating staff to specific units, also known as cohorting. Utilize overtime and long shifts for staff in the COVID-19 units to limit the number of staff needed. When possible, use staff who are immune (recovered) in the COVID-19 units. Prevent infected staff from working (except with COVID-19 patients) by tracking staff who are sick and testing for COVID-19, if possible, and keeping a log of who has had confirmed COVID-19.
Do you have a plan to prevent burnout?
Given the uncertainty regarding the duration of the pandemic, and with the promise of a vaccine still a year or more away, it is essential that healthcare workers can perform to their full potential over an extended period. This should include retraining clinicians and allowing them to practice to the top of their licenses in addition to strategies to enhance their wellbeing.
Can you provide mental health support for healthcare workers in this crisis?
While most of the population is socially distanced in the safety of their homes, healthcare workers, both clinical and support staff, are caring for patients with COVID-19, often without the resources required to do so safely. Lack of PPE, appropriate training, and staff has hindered their ability to save lives as they would normally. The morbidity and mortality of hospitalized COVID cases, coupled with the concern among healthcare workers that they themselves, their colleagues, or their family members may contract the contagion, have led to physical and mental exhaustion in the healthcare workforce.
At each facility, leadership needs to address the stress on individual providers and on general operations by monitoring reactions and performance, altering assignments and schedules, modifying expectations, and creating mechanisms to offer psychosocial support as needed.
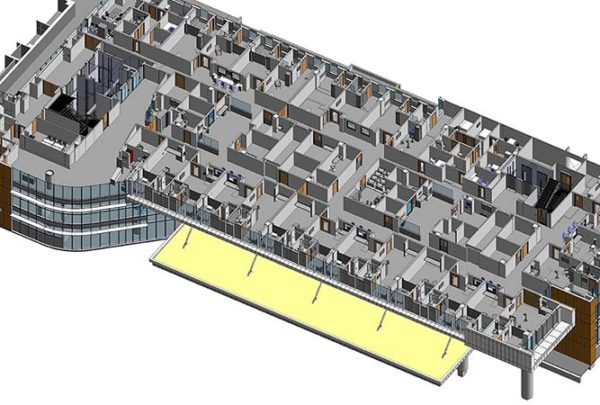
What approach should you take to restart deferred healthcare services?
Across the country, “elective” healthcare services in hospitals, outpatient centers, and physicians’ offices have been canceled or deferred to create capacity for COVID-19 patients, conserve PPE, and avoid exposing noninfected patients to the contagion circulating in these facilities. While this move is critical to halt the spread of the contagion and provide the necessary resources to care for patients, the impact has been financially devastating to most organizations and given rise to worsening conditions for patients who are unable to seek the care of their providers.
- Prioritize which services and/or procedures are being deferred, for how long, and with what consequences and create an alternative plan for patients who will be deferred. Create a process for refining and updating this plan as circumstances change, as well as a process to track deferred patients (see our tool Surgi IQ).
- Use your hospital data on COVID patients’ admissions, ICU census, ventilator use, ED admissions, or presentations to compare to pre-COVID levels of use to determine whether it is safe to begin reintroducing deferred patients back into the system.
- Develop a plan to begin a gradual resumption of services as the COVID-19 critical care demand subsides. A priority system for restarting deferred healthcare services must be developed in hospitals and the healthcare system.
- Utilize the AHA and ACS guidelines for resuming surgical procedures.
If current projections from health experts hold true, a second and maybe third wave of COVID-19 seem certain. We hope we have learned more about our capabilities and challenges over the past few months and are better prepared to respond, regardless of whether we still don’t know for certain its severity. It is imperative that decision-makers at hospitals, in communities, and at the state and federal levels do not delay in planning and preparing. With collaborative planning and sharing of resources, both human and economic, education and training could be started immediately. If we don’t and are just reactive, the human and socioeconomic cost of delays, coupled with the current impact from this first wave, will be massive.
Urban Report. (March 1, 2020) The Urban Report, Robert Wood Johnson Foundation, Hospital-Readiness Report. https://www.rwjf.org/en/library/research/2020/03/hospital-readiness-for-covid19-analysis-of-bed-capacity-and-how-it-varies-across-the-country.html
National Bioterrorism Hospital Preparedness Program. https://hbr.org/2020/04/how-hospitals-can-manage-supply-shortages-as-demand-surges?utm_medium=social&utm_source=twitter&utm_campaign=hbr
US Department of Health and Human Services. Pandemic Influenza Plan. https://www.cdc.gov/flu/pandemic-resources/pdf/pan-flu-report
Centers for Disease Control and Prevention. FluSurge 2.0. https://www.cdc.gov/flu/pandemic-resources/tools/flusurge.htm
Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Infection control. https://www.cdc.gov/coronavirus/2019-ncov/infection-control/index.html.
World Health Organization. Whole of Society Pandemic Readiness.www.2009-0808_wos_pandemic_readiness_final
OPENING UP AMERICA AGAIN Centers for Medicare & Medicaid Services (CMS) Recommendations Re-opening Facilities to Provide Non-emergent Non-COVID-19 Patient Care