One of the unintended consequences of the COVID-19 pandemic and extended lockdowns has been unused or ill-used office space resulting from employees working from home if their jobs don’t require them to physically be in the office. Now that we’re seeing a light at the end of the tunnel, companies are exploring options for employees to continue to work from home, either permanently or part-time. It’s too early to tell the long-term effects on commercial office buildings, but certainly fewer people will be making the daily commute.
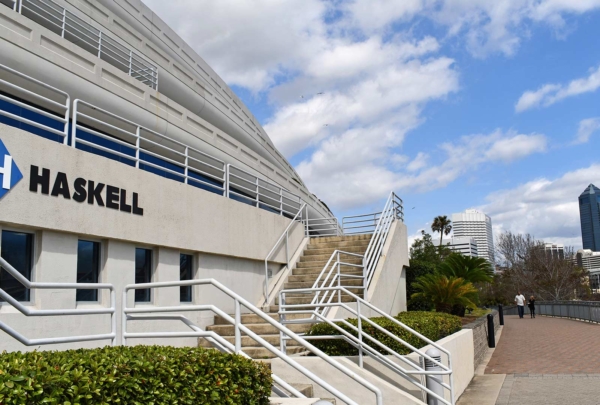
Health systems are not immune from this trend, especially with their administrative teams. When one health system elected to keep their non-clinical staff working from home, it opened a considerable amount of square footage in an owned administrative building, and it led them to question whether it could be repurposed into a revenue-generating clinical/medical office building. They engaged Haskell to conduct a rapid response asset planning exercise to evaluate not only which practices would be best collocated to create a center of excellence in the newly realized space, but to also reshuffle the rest of their physician practices within their remaining facilities and to advise regarding the long-term viability of those assets.
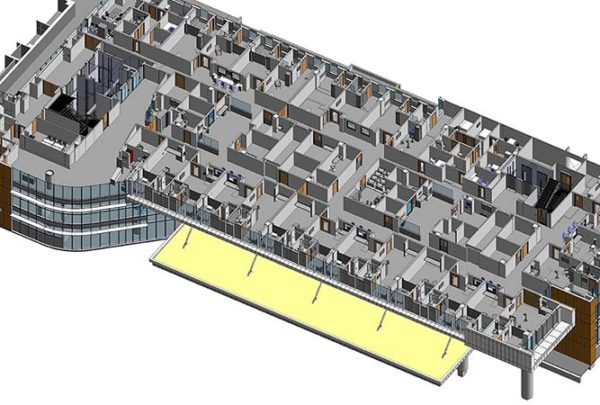
Using our Rapid Response Asset Planning tool, we embarked on a quantitative assessment of the client’s strategic initiatives for ambulatory service lines and facilities and the benefits and disadvantages of reorganizing, consolidating, or renovating their facility assets. The process involved on-site visits to each of the client’s locations to assess each building’s infrastructure, aesthetics, room quantities, and size compared with national benchmarks. Assessing a building’s infrastructure included evaluating the overall condition of its exterior envelope with regard to windows, overall insulation properties, and materials that need to be repaired. Infrastructure also includes the mechanical, electrical, plumbing, and fire safety systems. This can involve determining whether the electrical system has enough power to support proposed imaging equipment; for example, some older buildings, especially primary care clinics, were not designed to support the electrical needs to operate this equipment, so a more strategic approach is needed to determine whether repairs or upgrades are cost-effective to maintain the building as a long-term asset.
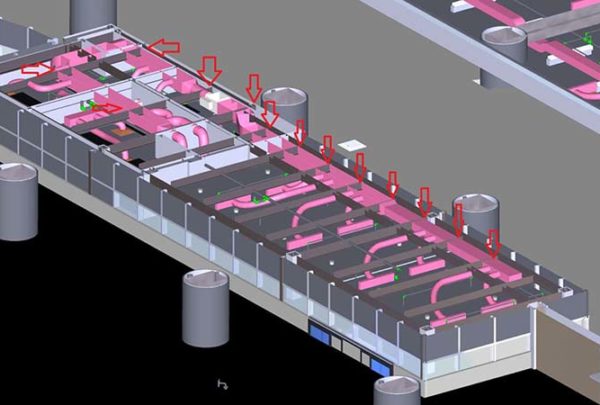
A major cost of any building’s operation is conditioning air, including heating, cooling, and filtration. Evaluating a building’s envelope and how well it is sealed and insulated will identify whether the HVAC system is operating efficiently or whether its performance can be improved to save on operational expenses. An assessment of air flow also encompasses entrances and vestibules to ensure air temperature and humidity can be controlled.
Exterior and interior patient accessibility is another critical component of a clinical facility. Facilities need to be located where they can best serve the community. Exterior accessibility includes assessing parking conditions, ease of parking, and navigating curbs and ramp access. In the interior of a building, access takes into account the patient’s journey to receive care: entry to the building and wayfinding to check-in, waiting areas and how they handle patient privacy, and access to exam rooms are all of concern. ADA requirements can also impose a large factor toward meeting building accessibility. Some older buildings are not ADA-compliant, so a facility assessment is warranted to ensure the building meets relevant codes.
Building accessibility also applies to staff. Team members must have easy access to and a sufficient number of supply and equipment rooms, and the location of physicians, nurses, physician’s assistants, and other staff relative to exam rooms must be taken into account. Location of these areas in relation to exam rooms can cause inefficiencies, which translate into longer wait times for patients.
A building’s aesthetics are an area that can be easy for the system to overlook, neglect, or not keep updated, but it’s true that outsiders will judge the quality of an institution and perceive the quality of the level of care they are receiving by how the facility presents itself. The asset planning process provides a perfect opportunity to make purposeful changes to an asset’s aesthetic and confirm it meets those of the overall system. A system can include a variety of assets, ranging from large medical centers to smaller clinics that often trend toward more residential materials and presentation. No matter the facility, all ideally have a harmonious look that showcases the brand so patients connect that facility to the larger health system. For example, signage across buildings needs to have the same font, color, and shape so people arriving know they’re at the right place. One of the benefits of conducting an asset review is that it provides a fresh set of eyes to identify issues that perhaps have been overlooked: stains on the building from water shedding, debris from trees, and tripping hazards in the parking lot and sidewalks, to name a few. Likewise, outdated or worn interior finishes and furniture can cause a bad first impression on patients and other visitors.
Evaluating space utilization and room size to meet current codes can help with deciding whether to invest in a facility for the long term. Maximizing square footage in some buildings could involve smaller renovations to create additional capacity. But additional capacity creates a need for additional support spaces. Staff members need workstations, supply closets, soiled holding, and toilet rooms to support additional exam rooms. When developing solutions for asset manipulation or movement, using benchmarks will ensure that support space is accommodated.
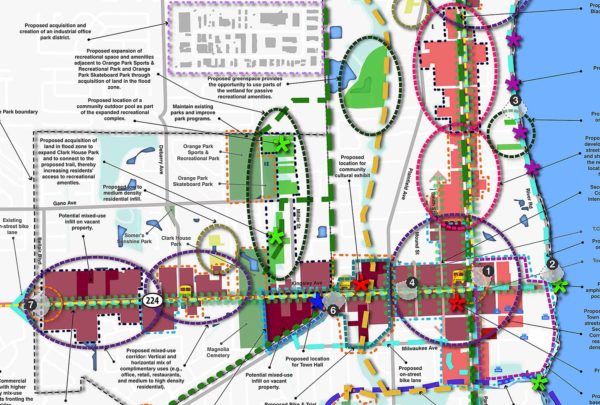
After completing the assessment, the next step is to map out where services could be collocated to benefit the community and perhaps create a center of excellence where practices can be consolidated. Inclusion of an estimate of total probable costs that incorporates construction costs, construction escalation, and relevant contingencies for each stage of the project, as well as a schedule for length of time needed for construction addition or renovations, is essential. The budget should include estimates for upgraded medical equipment or furniture that may need to be replaced in a 10- to 15-year cycle.
Our client was provided a tailored study outlining an actionable, efficient, and cost-effective implementation plan to not only best utilize their facility assets but more importantly serve their community of patients. The plan’s genesis emerged from their calculated response to a post-pandemic workplace.