My favorite find from our recent office move: A Magic 8 Ball. Even after being stored away in a back closet for over a decade, it still has all the answers (because we know all life’s most important questions can be answered by a plastic icosahedron floating in a black ball…).
Question: Will the hospital of the future be a majority ICU beds?
Magic 8 Ball Response: Don’t count on it
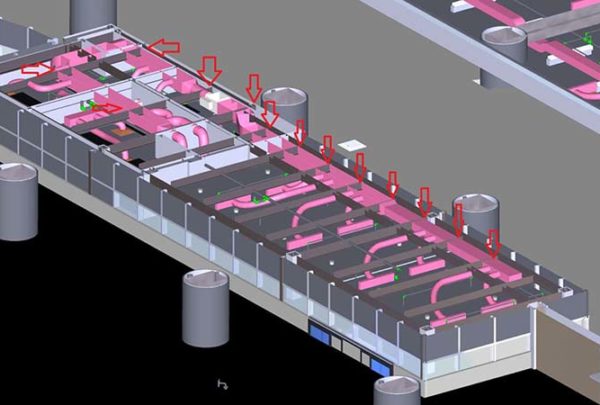
Haskell typically sees ICU patient days as a percentage of total days hovering around 7-15%. Despite evolving technological and clinical advances made to shorten recovery time and improve outcomes, we haven’t seen our clients’ inpatient acuity mix distribution change dramatically in hospitals that have kept their service offerings relatively constant.
In growth markets, however, we’ve had a number of clients with a need for additional ICU capacity. The need is driven by factors ranging from strategic service line growth to inappropriate utilization of ICU beds. Inappropriate ICU utilization is an area of increased focus as staffing and construction costs continue to rise and as policy changes tie reimbursement to outcomes.
The main driver of unnecessary ICU utilization is clinician preference or fear of moving patients to an intermediate care bed too soon. Often, if patients require care that isn’t critical but is more intense than a general medical/surgical (M/S) floor can provide, then providers will hold patients in the ICU. Instead, protocols and training should be in place to limit the subjectivity of patient placement.
We’ve also seen where capacity constraints on M/S floors sometimes ripple into ICU units and non-critical patients end up boarded in an ICU unnecessarily. In those instances, providers must identify the downstream causes of M/S capacity constraints. In some instances, the addition of an observation unit, or critical decision unit, to house observation patients provides a lower-cost alternative to inpatient bed capacity constraints.
Occasionally, the ICU serves as a “catch-all” for unique patient types like behavioral health or end-of-life. We know there’s is an inherent risk of infection with any hospital stay, but studies have shown that ICU stays increase the risk for hospital-acquired infections. Having the ICU serve as a “catch-all” puts patients at risk and is the costliest area to treat inpatients. The Society of Critical Care Medicine reports that ICU costs rose 92% between 2000 and 20101 and continue to rise.
Without reimbursement changes, the cost structure alone of a hospital with a majority ICU beds is not viable. The hospital of the future will still need step-down beds, general M/S beds, and observation beds to appropriately transition patients out of the hospital.
Question: Will the Magic 8 Ball go back into a closet for another decade?
Magic 8 Ball Response: Without a doubt.
Society of Critical Care Medicine – Critical Care Statistics https://www.sccm.org/Communications/Critical-Care-Statistics