Health systems, particularly complex areas such as the emergency and surgical services departments, have long used computer simulation modeling to understand the effectiveness of their processes and guide improvement and planning efforts. Right now, every health system and hospital in the world is trying to answer urgent questions about COVID-19 response planning, from how to best use available capacity, to how to make do with reduced staffing levels and equipment and materials shortages. Simulation planning can be the ideal solution to rapid planning and redirecting as needed as conditions on the ground change. Modeling can be as basic or as complex as needed to answer a particular question. There may be a misperception that building a simulation takes weeks or months to yield useful information, when in reality a useful simulation can be built in a matter of days, given the right inputs.
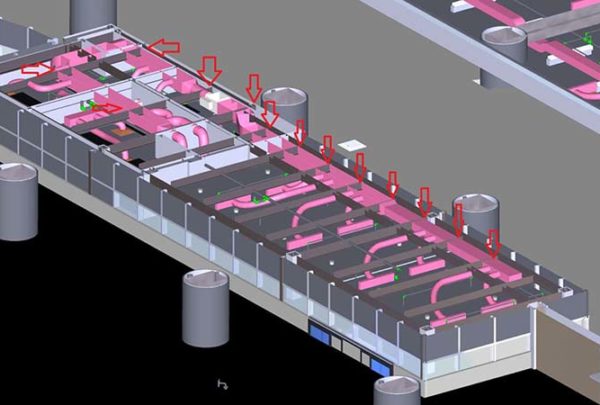
Although emergency departments and other areas of a hospital can have unpredictable utilization, planning of staffing, physical capacity, and other resources for patient care is possible; in most circumstances access is not totally random. Starting with a baseline of existing operations, an analyst can change inputs to a computer simulation model such as the rate of patients arriving per hour, the locations and length of time a patient needs to stay according to severity, and the availability of staffing or other vital resources required for care, to understand the effect those changes have on the system. For example, if an ED or hospital wants to know the impact of COVID-19 on its ED or ICU beds, a modeling exercise could give a range of potential scenarios and outcomes based on a worst-case scenario or for daily changes to resource availability, such as nurses or ventilators. Or if a hospital has set up drive-through testing clinics, modeling could help a team understand how many stations and staff are needed and how the process could work.
In my experience implementing computer simulation modeling studies, emergency departments have gone through multiple planning exercises for how to deal with patients who may have a contagion. The CDC’s H1N1 planning in 2009 triggered the need for separating triage stations and screening at the first point of contact with ED staff and to determine whether a patient was at risk for infecting others in the ED.[i] Then Ebola concerns prompted EDs to not only manage screening upon arrival but also the arrival into the department well before the door. For instance, many departments stationed staff outside both the ambulatory and ambulance entrances to ask patients about travel; if there was a potential exposure, staff would escort that patient directly to an Ebola-appropriate exam room that would allow staff to don and doff PPE and clear or prepare patients without contaminating the rest of the department. All these changes to process and impacts to resources and capacity were handily tested with simulation modeling.
With COVID-19, the likelihood is that in time, perhaps in a matter of days or weeks, EDs and hospitals will be overwhelmed with cases. Arrival of these patients will be the norm, and an ED and the rest of a hospital will need to understand how their processes and capacity will respond under extreme stress. This kind of surge planning has long been a staple in computer simulation modeling activities.
The above examples of simulation planning are extremely useful for understanding the impact of changing conditions in a single location. However, simulation planning doesn’t have to stay local. It can help a region calibrate capacity and resources during this pandemic. For example, if one hospital has regularly high ICU utilization, simulation modeling can help planners understand ahead of time where capacity can be used most effectively, considering transport times and impact to EMS, availability of other regional beds, and location and use of ventilators or other resources.
My prediction for the future is that health provider planning activity will not go back to a generally reactive state. Dealing with COVID-19 will prompt health systems with multiple hospitals in one region to work more closely together—to operate as a system—and share resources as needed on a regular basis. The pandemic may spur states to create systems and tools to proactively deal with community health threats, whether they are widespread seasonal surges or once-in-a-lifetime events. These state or regional systems, such as state health data exchanges that exist today, will gather data that can signal a potential threat and act accordingly on a large scale. Computer simulation modeling can be an effective tool in understanding how to mobilize resources to mitigate adverse impacts of these large-scale events by taking these early data points and combining them with known capacity and resources information.
Whether planning is local and specific or large-scale, computer simulation modeling can and will be a crucial and regular part of planning for community health.
[i] https://www.cdc.gov/h1n1flu/guidelines_infection_control.htm