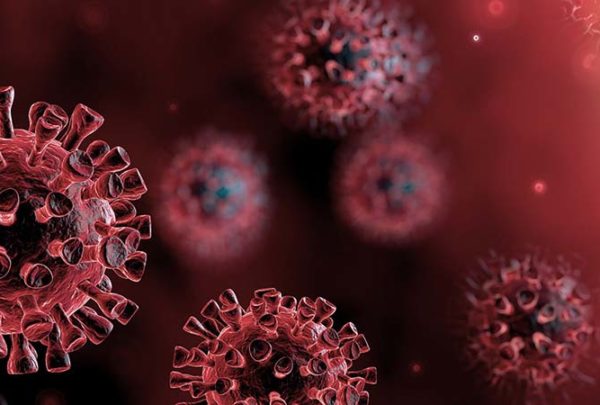
While emergency departments and critical care units have been inundated with patients due to the COVID-19 outbreak, many other departments in healthcare facilities have been shuttered to prevent the spread of disease to staff and non-infected patients. As state and local governments are preparing to slowly reopen the economy, hospitals are also beginning to restart the services, such as elective surgeries, that have been suspended.
The top priority when reopening is staff and patient safety. There are a number of steps you can take to create a safe environment for reintroducing programs that have been reduced or closed during the COVID pandemic as well as reintroducing patients and staff to environments that were previously less active.
Infrastructure
Plumbing systems need to be cleaned. Run faucets simultaneously for five to 10 minutes and flush toilets to confirm proper function.
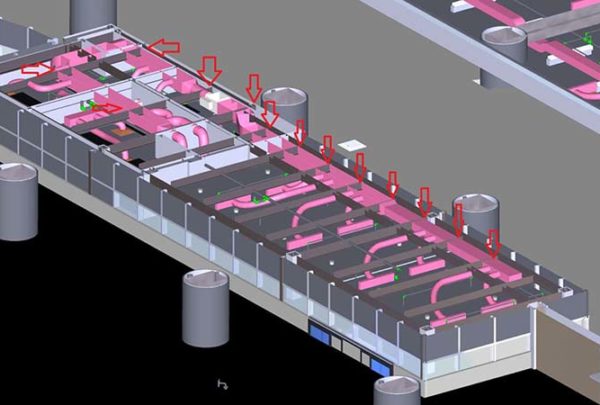
For HVAC systems, it’s important to temporarily or permanently change filters to HEPA filtration. This can be especially important when a unit has been serving COVID patients and is being converted back to non-COVID patient use. In areas that were not previously treating COVID patients, temporarily change filters to low pressure drop HEPA filtration.
- Run the unit on economizer to purge the system prior to opening the department, especially if AHU is serving an area with COVID patients and area being reopened.
- Run an AHU performance evaluation to confirm function prior to reopening the department.
Enhanced Safety
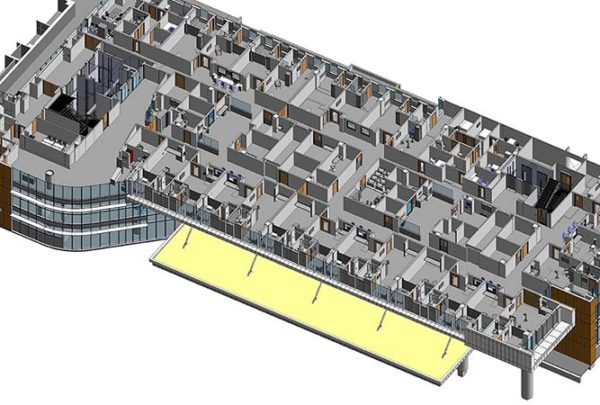
One way to improve patient and staff safety is to minimize waiting rooms. This provides an opportunity to control visitation and limit non-patients in the department. Changes to visitation policies may be necessary with signage to reduce traffic within a department. Increased control over department access could lead to an increase in security presence on site (operational/staffing change). Institute screening process for access to department for visitors.
Another way to possibly decrease cross-contamination is to reduce the number of high-touch areas, such as water fountains. Consider integrating touch-free water access for visitors.
Locating PPE stations throughout your facility provides an opportunity to add handwashing stations and hand sanitizers at department and facility entry points. Consider providing handwashing station in the waiting room.
Other considerations include:
- Conduct terminal cleaning of department prior to reopening.
- Add EVS supply storage in or adjacent to department for enhanced cleaning requirements to maintain safety.
- Consider a conversion opportunity for waiting space or other public spaces that are reduced in use.
- Reduce physical touchpoints:
- Integrate staff–dedicated handheld devices (tablets, laptops, WOWs, etc.) to minimize shared computer terminals
- Increase signage to encourage handwashing/sanitizing and minimize contact and to direct visitors for handwashing process and accessing departments.
Operational Enhancements
- Operational enhancements also can help increase staff and patient safety when your departments reopen.
- Potential for additional screening security staff to control access to the department and/or facility.
- Ramp up EVS staff to accommodate enhanced cleaning needs throughout the facility.
- Ramp up equipment cleaning capabilities for the equipment servicing patients between infectious areas and non-infectious (reopened) departments.
- Opportunity to dedicate mobile medical equipment to a department to minimize transporting equipment throughout the facility.
Patient placement will be critical to minimize placing infectious patients on the same units with non-infectious patients. In smaller facilities separating patients by unit may not be a viable option; therefore, consider co-locating patients within the same unit by corridor to minimize crossing patient traffic paths. Consider pretesting patients prior to placement to confirm appropriate location, and consider dedicating staff to specific units to reduce travel between infectious and non-infectious areas of the facility.
Patient transport will be important. Corridors to separate transporting infectious vs. non-infectious patients would be a significant undertaking, so an alternative might be PPE for the patient during transport and/or scheduling transports to minimize patients bypassing each other.