Ambulatory centers have been touted as convenient locations for patients to take care of clinical, diagnostic, or other care needs away from an acute care hospital, where services may be costlier and more difficult to access.
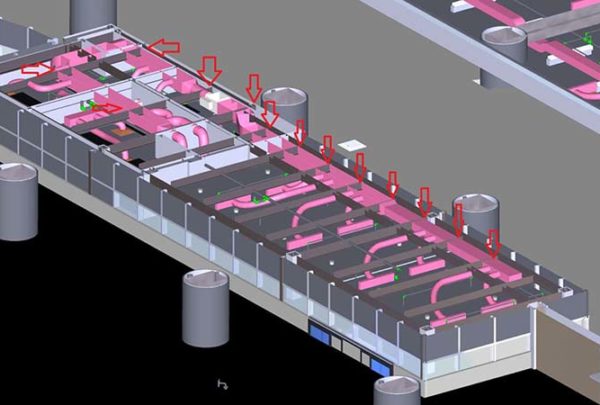
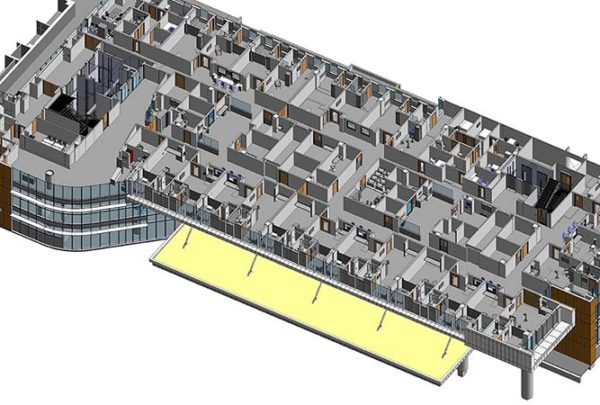
To provide the best care delivery model and ensure high patient satisfaction, designers have to be thoughtful about incorporating the right architectural elements into what is often limited square footage. A rigorous analysis that may include patient journey mapping, patient-level clinical and operational analysis, functional programming, and computer simulation modeling must be used to inform the architectural planners of the best use of space for efficient workflow and patient experience. Below are a few examples.
Physician Clinics
From an architectural perspective, it’s becoming a luxury for physicians to have space dedicated solely to his or her practice. Square footage designated as private office space may be occupied for only a short time and could be better used as clinical space within the practice area. Alternatively, square footage adequately appropriated for team space improves communications regarding patient care. For example, nearby equipment and supply storage can reduce staff travel time and time spent looking for items.
Similarly, a physician or midlevel provider may not need to have dedicated exam rooms (i.e., 2-3 per provider) if the exam rooms are properly configured and outfitted flexibly enough to support several providers at once. Specialists may share exam space from one day to the next or even during the same shift, along with flexible procedure and support space such as equipment storage.
It’s important to note that extensive planning and due diligence must go into designing this space. Analytical tools such as patient journey mapping, computer simulation modeling, and functional programming can ensure that both designers and practitioners are aware of and agree on how the space will operate and what will happen under different operating conditions such as volume increases or variation in specialty visits.
From the patient perspective, the goal of many ambulatory centers is to provide co-located services that patients may typically need on a single visit, such as clinic, lab, and imaging services, to reduce travel and wait time. Patient use of these services during a visit dictates the most appropriate adjacencies that the architect will design.
However, technology must also support this close connection. In a multi-practice facility, each area must be electronically connected to allow for arrival alerts, patient status notifications, results and records sharing, and other messages that can facilitate a visit with little waiting. By tracking the operational and data flow from a patient’s perspective, the ambulatory center can best determine clinic adjacencies as well as information system requirements.
Pre-Op Testing
In many clinics, the different functions of pre-op testing are performed in separate spaces, so providers struggle with the ebb and flow of patient volume not aligning with each available, specialized room. One solution Haskell found was to implement 10 multifunction rooms, supplemented with portable equipment, rather than five EKG rooms, five lab rooms, and separate dedicated exam rooms. If each room can accommodate all functions, the spaces can be used by any staff member at any time, for any patient. Providing this flexibility can usually reduce the overall number of rooms being provided.
Surgery
With any surgery project, Haskell studies the patient flow from entry to prep before surgery to surgery to post-op. Because prep is usually conducted in the morning and recovery in the afternoon, a single area composed of like rooms can often be used for both functions. However, if a surgery schedule changes to better level-load the operating rooms such that more cases are scheduled in the afternoon, then the flow of both pre- and post-op functions can affect available capacity of this area dramatically. Knowing how to schedule fluctuations affect the use of patient spaces is crucial for planning and designing these spaces. Computer simulation modeling of these potential schedule differences can provide a wealth of information to planners.
Summary
The rigorous analytics that the Haskell operations team provides to architectural planners is critical to the success of facility planning. The team’s process ensures workflow and patient experience are maximized.
In Part 2: Eliminating certain types of spaces altogether and focusing on implementing efficient processes can substitute for adding some types of space.