I’m on a campaign to remove hallway beds from emergency departments across the country. Perhaps this seems like an unorthodox idea, but three factors convinced me that hallway beds do not belong in the ED.
1) Adding more capacity in the form of hallway beds typically increases LOS because it creates more places to “store” patients, often without a corresponding increase in staff to move them through the process.
Granted, with additional open beds staff can initiate treatment for more patients and empty the waiting room. However, doing so reduces or eliminates the sense of urgency since no patients await care. That’s when processes may slow down.
One can understand why a charge nurse would make the decision to place a waiting patient in a hallway bed—the capacity exists. But are staff available to care for that patient?
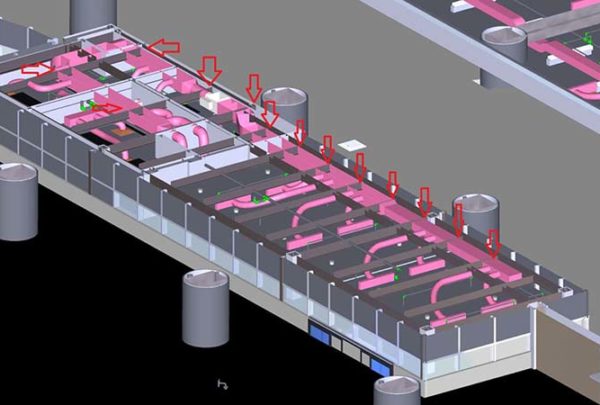
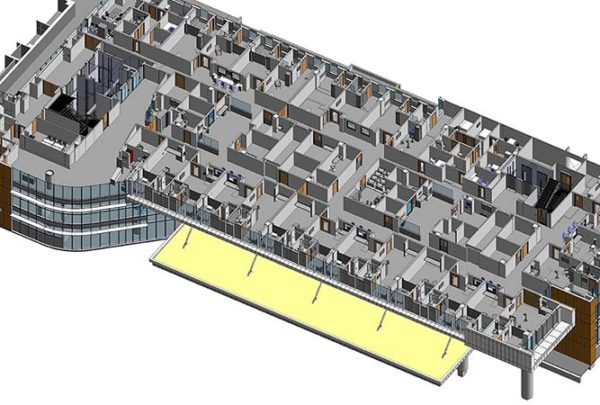
For those who maintain that having more beds will solve all problems, we use computer simulation modeling to validate both the appropriate number of spaces and the ideal process flow. We can virtually test changes before making them, testing multiple variables independently or in combination with one another.
First, we execute one scenario that adds as many new beds as can possibly be added. For comparison, we execute a second scenario using the existing physical space, and changing only operational processes. When focusing exclusively on additional capacity, the simulation model shows that length of stay will go up in nearly every case. Conversely, when we focus solely on process change scenarios and make no change to capacity, length of stay improves.
2) Whether the hallway bed is an additional assignment on top of a nurse’s existing workload, or staffed as part of a nurse’s regular assignment, LOS increases when a nurse’s patient load increases.
Haskell has found that a staffing ratio of four beds to one nurse works better than other ratios. This means that even if you could put five beds in a fast track area, for example, you may find that four would have worked better — because the fifth one is simply difficult to staff.
From a quality of care standpoint, a nurse who cares for four patients delivers better care and has more time at the bedside than an overtaxed nurse who cares for six patients. It comes down to understanding your resource capacity and matching the number of beds to staff resources. For those who counter that budgets may not allow staffing to a four patients to one nurse ratio, then continually focusing on process improvement becomes even more important, so that reductions to length of stay ultimately curtail bed demand.
3) Removing hallway beds can actually decrease LOS, because staff have no choice but to turn beds over faster.
I just completed a series of computer simulation models showing that removing seven hallway beds from an existing environment actually improved LOS overall for all patients. Without hallway beds to increase available capacity, staff proactively discharge patients to make beds available for incoming patients. This is best practice anyway.
- Prioritize the discharge of patients out of the ED, not when you need the bed, but beforehand.
- Move a stable, upright patient out of a bed (to a subwait area, if available) after completing evaluation and testing. Conduct discharge either in a bed or other private area.
- Make it everyone’s job to ensure that patients are fully registered before delivering discharge instructions.
Some suggestions to smooth the transition:
- Start by removing one hallway bed the first week, another bed the second week, and so forth.
- Try another process change simultaneously. For example, pair moving patients out of the system faster with getting patients into the system faster. As patients arrive, forgo triage at the front and instead send them directly to an available bed. Stopping at the creates a queue that compounds delays throughout the day.
- Seek out patients to discharge, and discharge one patient before taking on another.
If we know that simply adding capacity without appropriate resources will increase LOS, it follows that removing beds could potentially decrease LOS, make staff more productive, and improve the quality of care.