If you don’t know for certain that a process change will work before you try it, you’re guessing. People guess because it’s easier than looking at data. Or because they have anecdotal evidence. “That transporter is always late and I have to take the patient myself!” Unfortunately a lot of anecdotal evidence just yields red herrings. It may not point to the root cause of problems.
Guessing wastes time
The Goldilocks approach means you work first through “too hot” and then work through “too cold” before you get it “just right.” The approach takes time, which equates to money, neither of which is in abundance.
Guessing increases risk
Guessing makes your staff and patients the guinea pigs of your experiments. Healthcare in general is expensive. We also know that designing or redesigning space, process, or IT in healthcare is expensive too. When something is expensive it’s best to try it before you “buy it”. In this case, test it before you build it or renovate it or improve it.
You’ll have these opportunities to guess (or preferably, not guess)
In the next twelve months, you will likely encounter one of these scenarios:
- Management has given you faster throughput goals. Will you use trial and error to see which changes will meet the new goals?
- You are at the beginning or in the middle of a renovation project. What is the best way to function to continue to provide excellent care? What processes need to change, what is the most efficient staffing model? How will your metrics change and what can you do to keep them from deteriorating?
- Your patients wait too long for test results or discharge. How will you decide the best course of action to improve wait times?
- You are certain you need more space in your department: more treatment rooms, more storage, more charting area. How do you prove it? What if what you really need is better workflow and patient flow? You can change processes a lot faster than you can change architecture.
- You are short on staff. Could you be more efficient with the same staff? Would team staffing work? Mid-level providers? How can you prove it will work?
Building mock-ups and trialing process in situ are great, if you have extra time on your hands and an open-minded staff. But often you need to be able to prove that something will work. You may analyze the data and figure out a new process that seems so obvious that it HAS to work. But without some kind of analytical model to test the new design or process, you are still guessing. It may be an educated guess. But it’s nearly impossible to consider every connection between the current and proposed state.
Computer Simulation In Healthcare
Computer simulation modeling can do this and test scenarios before you make a costly change. Most industries use simulation modeling to test aspects of their processes and designs. For instance: it’s too expensive to create a suboptimal manufacturing line. The consumer products industry uses computer simulation modeling all the time.
Yes, it’s orange juice, rather than life and death on the line. If low-risk manufacturing processes warrant computer simulation modeling, why not healthcare? Given the variability of human behavior, the rapid analysis of millions of scenarios would greatly benefit caregiving models. Shouldn’t patient care be at least as worthy of study as juice?
How do you know?
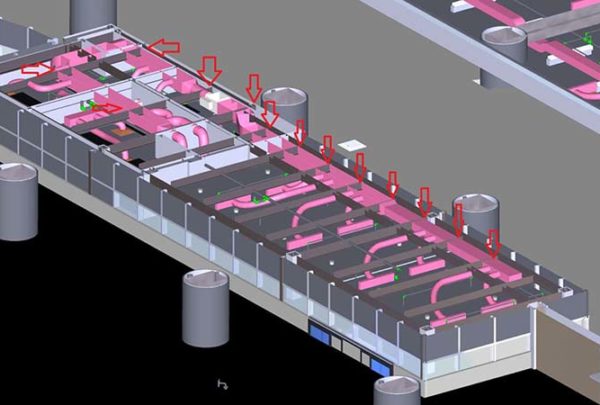
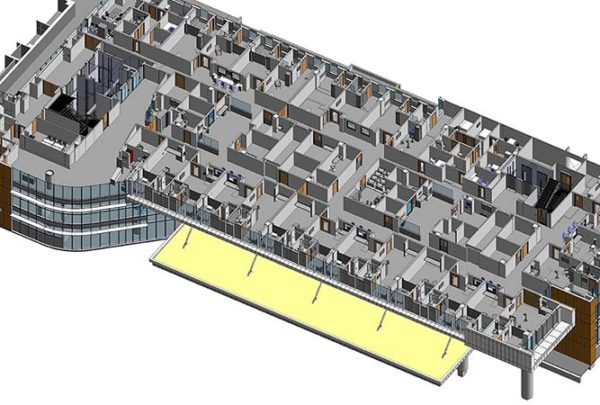
A good simulation model should allow you to quantify your current conditions. You may find issues, bottlenecks, and constraints where you didn’t expect them. The model will also validate and quantify issues you’ve known for a while. A baseline model that includes a staffing model, physical design and process flow is ready for testing options.
Change the physical design, change the operational processes, change staffing models. Change pieces and parts of all these simultaneously or individually. The model can test physical capacity, one or more staffing or process improvement ideas, and combinations to determine impact before making changes or assumptions. Often the end result is greater than the sum of the parts.
Try the reverse! Start with a goal for throughput, as an example, and see what changes are necessary to meet that new goal. You may find that you can do better than best practice.
A good simulation model uses your department’s specific processes, data, and current physical design. You know your current design, and you can observe and document your processes. You can easily get valid data from your information system. Or, if you don’t have one, from patient charts and staffing grids. With the right computer simulation expertise, you can have a baseline model up and running in a few weeks.
Here’s some examples of current challenges and what your new life will look like with computer simulation modeling.
- Administration: “Your new throughput goal is 25% less than current.”
Future You: “No sweat. I will use simulation to prioritize what to do first and the outcomes we can expect from each improvement. I will know how to proceed in a couple of weeks.”
- Administration: “We’re renovating your department. Be sure to continue to maintain the same level of care and patient satisfaction scores.”
Future You: “Bring it. I will use the simulation model to test each phasing option. Based on the one that generates the best results I’ll create processes and staffing models that ensure the waiting room volume stays low. And that door to physician and lengths of stay don’t increase.”
- Administration: “You need to shorten the length of time that patients wait for test results or discharge.”
Future You: “I have quantified that patients who are ready for discharge stay too long in the department by 45 minutes on average.”
- Present You: “I need more space, more treatment rooms, more storage, more charting area.”
Future You: “Ok I can use the simulation model to test how many spaces of each I really need relative to operational flow. I can show that changing processes will make up for a lack of treatment spaces in the short term. I can also test how long the improvements will hold and show how long before I really need to escalate the urgency.”
- Present You: “I am short on staff.”
Future You: “I can use the sim model to test various staffing models even by day of the week. I can add or subtract staff to test different models of care: team staffing, mid level providers, or the use of transporters. Then if I really need staff, I can say that the consequence of being short two techs is an ALOS thirty minutes longer than with two techs.”