As we define our new normal based on our COVID-19 experience, each of our perspectives will begin to shape healthcare design and preparedness for years to come. Our healthcare systems are already under a microscope and feel tremendous pressure from their communities to make changes to be more prepared, accommodate surges, and by the way, keep the cost down. Based on what we have learned so far, even though the data is still maturing, we can begin the discussion on planning and understanding the options.
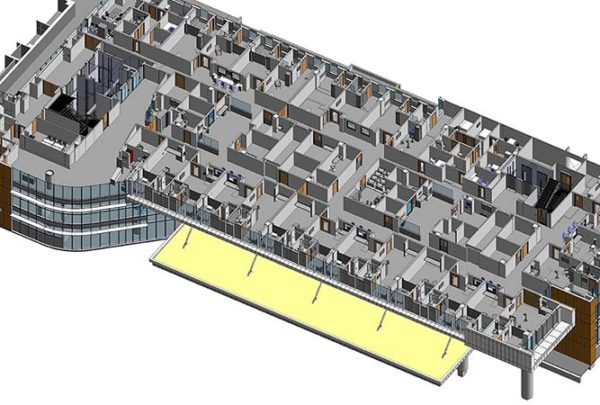
In light of this pandemic, the lack of ability to isolate a surge volume of airborne disease patients is evident. So how do we accommodate that effectively and remain practical in facility construction as we move forward? The ability to convert from positive (or neutral) pressure to negative pressure seems the most promising option; however, it is not as straightforward and simple as one may think. Hospitals are generally designed neutral to positive pressure in patient-care areas, and similar to the human body the balance of a hospital’s infrastructure systems is essential to its function. Reversing the operation of parts and pieces can disrupt other areas with unintended consequences. Therefore, the implementation of negative pressure operations needs to be carefully evaluated comprehensively.
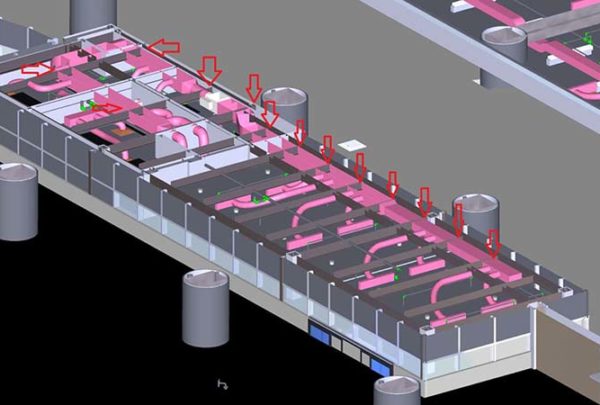
Increasing a facility’s complement of Airborne Infection Isolation (AII) rooms versus negative pressure patient rooms are two seemingly similar solutions with each posing varying levels of tradeoffs of risk and complexity of design. Each of these room types by definition ideally exhausts its airflow to the outside in a safe manner, and for new construction of AII rooms there are no exceptions but to exhaust this airflow. AII rooms additionally impose strict requirements over negative pressure with respect to pressure differential and significant air change rate requirements. Depending on the quantity of rooms desired, it may or may not be possible or energy efficient to maintain AII requirements year-round with the current infrastructure. Conditioning additional outside air to compensate for the increased exhaust required (Option #1) likely requires larger or supplemental HVAC equipment, additional chiller capacity, increased power feeds, and many additional components to make the selected configuration operational.
There are exceptions in the FGI Guidelines for renovations that allow recirculation through HEPA filtration as an (Option #2) if exhausting is not practical. Fan-powered HEPA filtration units can be used in these applications, tying into existing ductwork and BAS systems to achieve not only flexibility converting to negative pressure but AII-compliant air change rates. But it must be considered that while HEPA filtration is 99.97% effective, exhausting fugitive air is the most certain at the prevention of cross-contamination and reduces risk associated with maintenance/testing of HEPA filters effectiveness.
Hospital areas with the ability to exhaust air directly outside, via accessible exterior walls or pathways for additional exhaust ductwork, can pursue an option of HEPA filtration and partial exhaust as option #3. Exhaust in these spaces can be maximized to the extent the existing HVAC system can absorb the load and HEPA filtration units. Each of these HVAC options is not absolute and, depending on the quantity of rooms determined, operational requirements and existing conditions may require variation. It is also important to note that with any configuration additional measures can be incorporated to increase sanitation: UV light, vaporized hydrogen peroxide, bipolar ionization, or simply maintaining proper humidity levels (40%-60% RH).
Based on what we have learned from COVID-19 and until healthcare systems perform risk assessments with this new data to determine their calculated position, it is unclear what exactly the best solutions may be. Prior to COVID-19 our experience informed us that our AII room ratios were relatively sufficient for normal operations. However, these ratios are insufficient when responding to a pandemic. Solutions to address future airborne infections range based on a hospital’s threshold for risk in normal operation as well as during an event such as a pandemic.
An impractical solution would be renovating or building numerous additional AII-compliant rooms that will be unnecessary during normal operation. These rooms would incur additional capital and operating expenses during normal operation.
A more practical solution would be renovating or modifying for flexible operation, both observation rooms and an identified patient unit for infectious control. Normally they would operate at neutral or positive pressure until required. An observation room would be the first line of defense; if a patient is suspected of airborne infection risk. Then as needed the room could be converted to increase HEPA recirculation and become negative. A patient unit could have similar functionality for all the rooms until called upon. To a lesser degree, a quantity of AII rooms could be added as well, but the option would depend on the Infection Control Risk Assessment (ICRA) of the facility and the existing system servicing the space.
Design and engineering solutions are vital for addressing and treating patient surges during a pandemic. But as part of the risk assessment, hospitals need to evaluate protocols for normal and pandemic operation, including the separation of patients, triage, patient transportation, and the supply chain.
To learn more about how the pandemic could affect patient room design, read “Increasing the Capacity of Airborne Infection Isolation Capable Rooms.”