Centralized care is emerging to reform patient care operations by generating real-time, actionable analytics and proactive recommendations. This revolutionary technology uses the traditional hub-and-spoke model to enable providers to track patient progression based on their clinical condition, ensuring patients are transitioned to the most appropriate care location.
As healthcare providers rethink their approach to capacity management, they are looking to unite stakeholders across campuses, facilities, and departments with data from throughout the network. By building out Command Centers that combine a variety of technologies in strategic ways, healthcare systems can provide a holistic view of their data in real-time.
When deployed and utilized effectively, Command Centers can provide healthcare organizations operational insight into their systems, allowing cross-collaboration and enterprise-wide visibility. Utilized as a centralized hub to empower a caregiver team, organizations can provide coordinated care across their systems, expand patient access, and continually improve outcomes. However, deploying Command Centers incorrectly or implementing to solve the wrong problems can be costly.
Why Command Centers?
Command Centers have evolved over the last two decades from focusing on throughput and security to incorporating operational analytics for quick decision-making on care delivery and improving overall efficiencies and outcomes. They now include processes such as analytics, dashboards, equipment monitoring, telemetry, supply chain and bed management, environmental services, security, and facility information. The Command Center team uses predictive analytics and scoring systems to determine which patients are sicker and which have an actual discharge barrier. All Command Centers enable health systems to make full use of available capacity and improve resource utilization.
Shift in Focus and Prioritization
The need for Command Centers is propelled by the necessity for hospital CIOs to develop transformational strategies and move away from departmental cost centers. The approach is shifting, and today CIOs are becoming partners in the hospital’s business strategy and enablers of business growth with digital transformation leading their strategy. This evolution is putting pressure on the CIO to modernize the IT business — and to do it fast.
Each Center Is Unique and Different
Coupled with artificial intelligence and machine learning, much of the data analysis and decision-making are done by human workers, leveraging technology to comprehensively see their entire network, across multiple campuses and facilities, often statewide. There are a few different models to organize enterprise-wide Command Centers, and once you’ve seen one … you’ve only seen one, as they vary in purpose, organization, and execution.
Hub and Spoke
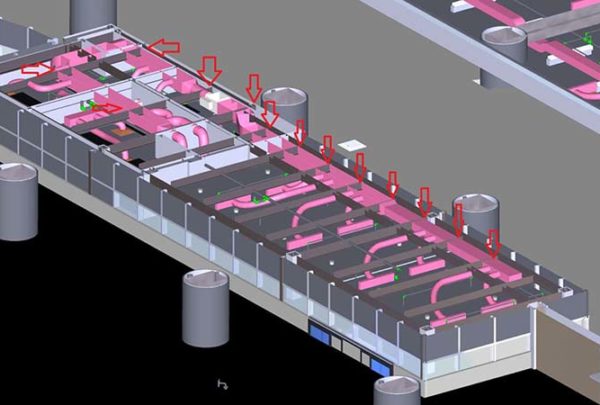
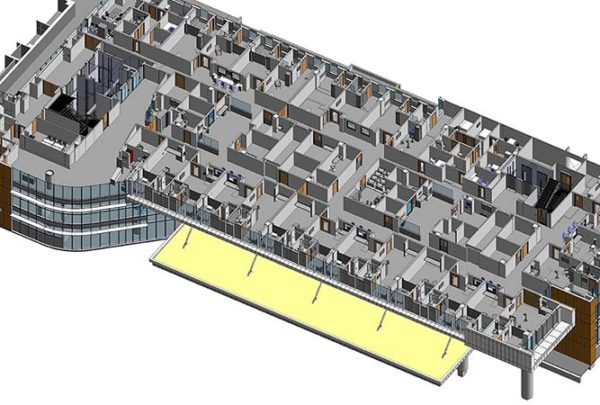
The Hub-and-Spoke Command Centers co-locate people, processes, and technology into a single physical space to leverage collaborative decision-making and workflows, facilitating the improvement of patient throughput throughout the system.
Multiple Hubs (Regional)
For larger multistate or geographically dispersed systems, multiple Command Center hubs are established for regions. Their associated spokes, located on smaller community and/or medical outpatient campuses, are directly connected to the regional hubs (typically tertiary centers). The data is then compiled and reported to a main hub, often located on the system’s flagship campus or sent to the system’s corporate location. The idea is to break down the aggregate data and management into actionable items for quick decision-making and execution based on local market and organizational dynamics.
Location-Specific
Establishing Command Centers can be specific to departments and/or service lines and implemented on a smaller scale to address and manage a specific challenge or issue. We typically see these established within surgery, diagnostic services, establishing interventional platforms, and managing regional emergency/incident command services.
Data Integrity, Interdependencies, and Operational Efficiencies
Command Centers also provide insight into some of the most complex areas of health systems. These include departments and/or service lines that have historically been difficult to understand because of the dynamics with those departments, the invasive nature of patient care that is provided, and the complexity and interplay of all the processes and resources needed to support the care provided.
Because of these challenges, most providers have focused on the patient care aspect (experience and outcomes) and not the operational complexities. As a result, the operational and financial data coming from these departments are incomplete, have gaps, or are recorded incorrectly. This poses a huge threat to a successful implementation of a Command Center since accurately capturing the operational flow of how the patient moves through these areas, how staff are assigned, how physicians are utilized or assigned to patients, how procedures are booked, and how resources are allocated are critical data points to successfully realize the Command Center’s capabilities.
It is crucial that clinical departments like the following are assessed for data integrity and operational flows early in implementation or prior to initiation:
- Surgery
- Cath. Lab/IR
- GI Lab
- Imaging
- Emergency Department
- ICU/Stepdown Beds
- Sterile Processing
Focus on Becoming More Proactive
By increasing the use of advanced analytics into performance improvement initiatives, simulation models of patient flow are mapped in hospitals, hospital networks, and outpatient facilities. Based on what is happening in the market, Command Centers can test possible changes in beds, surgical schedules, staffing models, and costs based on various growth and care model scenarios. This allows providers to plan for possible volume peaks and potential diversions. From admission data to operating room schedules to patient movement tracking, mission-critical technology can be applied in myriad ways to improve patient care across the system.
A successful Command Center needs to integrate clinical status with optimized and efficient flow management to make timely and appropriate operational decisions. Decision-makers can then allocate the most appropriate resources to keep costs down, grow patient volumes, and keep their system performing at peak levels.